
Prolistem® at the ESHRE 41th – Paris
We are proud to have participated in the 41st Annual ESHRE Conference in Paris, a premier international event where the global reproductive medicine community gathers
Non-obstructive azoospermia (NOA) is one of the most challenging forms of male infertility. Unlike obstructive azoospermia, where sperm is blocked from being released, NOA occurs when the testicles fail to produce enough sperm due to medical, genetic, or environmental factors. While this condition can be overwhelming, understanding its causes can help in finding the best treatment options. In this article, we will explore the primary causes of non-obstructive azoospermia, diagnosis methods, and potential treatment solutions.
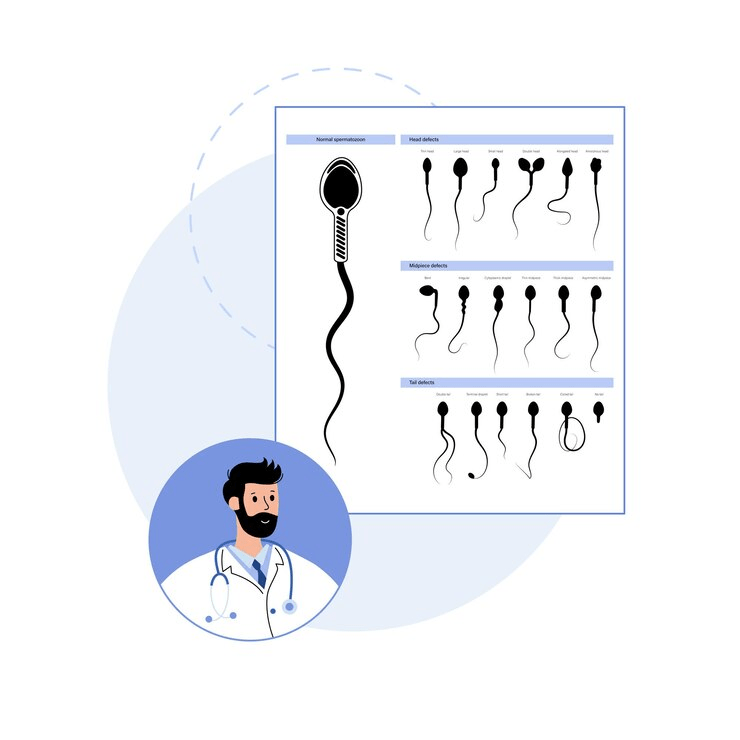
Azoospermia is the complete absence of sperm in semen, affecting about 1% of men and 10-15% of infertile men. It is classified into:
Several factors contribute to NOA, ranging from genetic disorders to lifestyle habits. Below are the most common causes:
Genetics play a significant role in male infertility. Some genetic conditions that contribute to NOA include:
Hormones play a critical role in sperm production. An imbalance in key reproductive hormones can cause NOA:
Some men with NOA have problems directly related to the testicles. These include:
Certain chronic diseases can interfere with sperm production, including:
Severe infections can damage the testicles and interfere with sperm production:
Unhealthy habits and exposure to toxins can also contribute to NOA:
If a man is diagnosed with azoospermia, the following tests can determine if it is obstructive or non-obstructive:
While NOA is a challenging condition, there are several treatment options:
If treatments do not work, couples have alternative options:

We are proud to have participated in the 41st Annual ESHRE Conference in Paris, a premier international event where the global reproductive medicine community gathers

Introduction: A New Era of Hope for Male Infertility The promising cure for azoospermia 2025 is redefining the future of male fertility. As medical science
Prolistem, a patented formula, has not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
PROLISTEM® is a Patented Formula
Copyright © 2025 Prolistem®