
Gene therapy for azoospermia treatment
Introduction Male infertility, especially caused by azoospermia, affects millions of men worldwide. For those suffering from non-obstructive azoospermia, treatment options have been limited. However, thanks
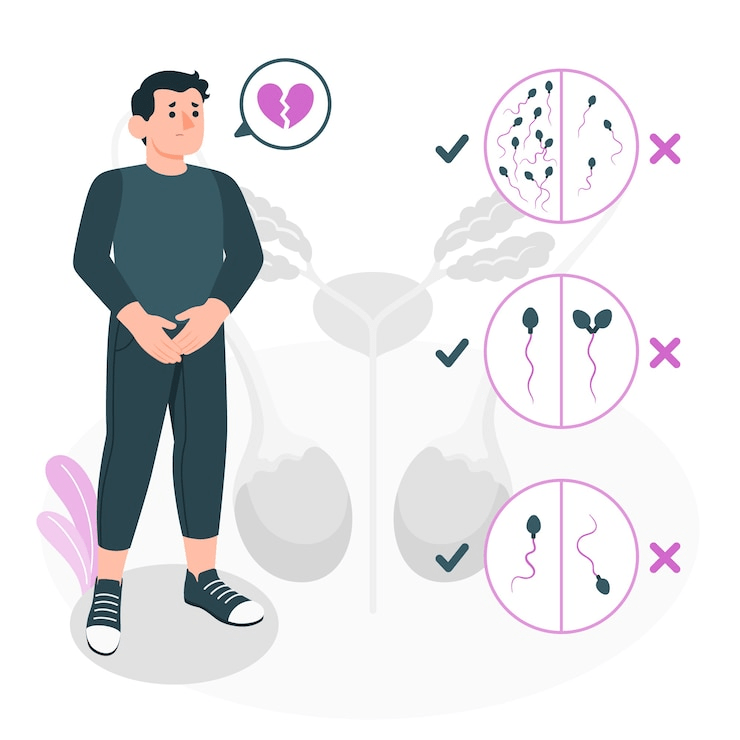
How Azoospermia is Diagnosed. Infertility affects millions of couples worldwide, and in about 40–50% of cases, male factors contribute to the problem. One serious male fertility condition is azoospermia, a situation where no sperm is found in the semen. Although it affects only around 1% of all men, the impact is significant.
If you or someone you know is dealing with fertility challenges, understanding how azoospermia is diagnosed is an important first step toward finding solutions. This detailed guide will walk you through the entire diagnostic process, explain why early diagnosis matters, and highlight what men can expect during medical evaluation.
Before diving into the diagnostic process, it’s essential to understand what azoospermia means. In simple terms, azoospermia occurs when a man’s ejaculate contains no sperm.
There are two main types of azoospermia:
Obstructive Azoospermia (OA): Sperm production remains normal in the testicles, but a physical blockage prevents sperm from mixing with the ejaculate.
Non-Obstructive Azoospermia (NOA): The testicles fail to produce sperm adequately, or production stops entirely.
Each type has different causes and treatment options. For this reason, proper diagnosis is crucial.
Identifying azoospermia early provides several benefits. For example:
It allows doctors to discover reversible causes.
It gives couples more time to explore treatment or fertility preservation.
It reduces emotional stress through clarity and guidance.
It improves the likelihood of retrieving sperm for assisted reproductive treatments.
With that in mind, let’s explore how azoospermia is diagnosed step by step.
A semen analysis is the first and most essential step in diagnosing azoospermia. This simple lab test gives doctors crucial information about male fertility.
The lab evaluates several aspects of the semen sample:
Sperm count
Sperm motility (movement)
Sperm morphology (shape)
Semen volume and pH
Presence of white blood cells or debris
During this test, a technician examines the semen under a microscope. If no sperm are visible, the lab will often spin the semen in a centrifuge to concentrate any cells that might be present. This step improves detection accuracy.
To confirm azoospermia, doctors recommend repeating the semen analysis at least twice. That’s because temporary issues—like stress, fever, or improper sample collection—can lead to false results.
After confirming azoospermia, the next step involves a detailed physical examination and a thorough review of your medical history.
Size, shape, and firmness of the testicles
Signs of a varicocele (enlarged scrotal veins)
Any lumps, abnormalities, or scars
The presence or absence of the vas deferens
Ejaculation problems or low semen volume
Doctors will ask questions about your:
Past infections like mumps
Exposure to chemicals or radiation
Injuries to the groin area
History of surgeries or medication use
Lifestyle factors such as smoking or drug use
These clues help identify whether the azoospermia is likely caused by a blockage or a production problem.
Hormones play a vital role in sperm production. Blood tests allow doctors to evaluate your endocrine function.
FSH (Follicle-Stimulating Hormone): High levels usually suggest a sperm production issue.
LH (Luteinizing Hormone): Helps regulate testosterone.
Testosterone: Low levels may signal testicular dysfunction.
Prolactin: Elevated levels could indicate a pituitary tumor or imbalance.
Estradiol: Imbalances can impact male fertility.
For example, high FSH combined with low testosterone often indicates non-obstructive azoospermia. On the other hand, men with normal hormone levels and a low semen volume might have obstructive azoospermia.
By analyzing these results, doctors can better determine the cause and choose the right treatment path.
If azoospermia results from sperm production failure, genetics could be the underlying cause. Genetic conditions account for up to 15% of non-obstructive azoospermia cases.
Karyotyping: This test checks your chromosomes for abnormalities such as Klinefelter Syndrome (47, XXY).
Y Chromosome Microdeletion Test: This test looks for missing parts of the Y chromosome, particularly in regions responsible for sperm production.
CFTR Gene Testing: Men born without vas deferens often carry mutations in the CFTR gene, which is also linked to cystic fibrosis.
It explains the root cause of infertility.
It helps doctors predict whether sperm retrieval might be successful.
It determines if the condition could be passed on to future children.
Understanding your genetic profile helps guide your fertility treatment options more effectively.
When doctors suspect a blockage in the reproductive tract, imaging studies provide more information.
Scrotal Ultrasound: Checks for tumors, varicocele, or other abnormalities in the testicles.
Transrectal Ultrasound (TRUS): Looks at the prostate and seminal vesicles to identify blockages in the ejaculatory ducts.
MRI or CT scans: Used in rare cases to investigate deeper anatomical problems.
These imaging techniques offer a clear view of the structures involved in sperm transport and help confirm whether a blockage is present.
If test results remain unclear, a testicular biopsy provides the most direct answer.
A surgeon removes a small sample of tissue from the testicle. A specialist then examines it under a microscope to check for sperm cells.
It confirms whether sperm production is occurring.
It distinguishes between obstructive and non-obstructive causes.
It allows doctors to collect sperm directly for use in IVF with ICSI (Intracytoplasmic Sperm Injection).
In many cases, even when no sperm appears in semen, doctors may find a few viable ones in the testicles.
Diagnosing the type of azoospermia leads to better treatment planning. Here’s a comparison:
| Feature | Obstructive Azoospermia | Non-Obstructive Azoospermia |
|---|---|---|
| Sperm Production | Normal | Impaired or absent |
| Hormone Levels | Usually normal | Often abnormal (FSH ↑) |
| Testicle Size | Normal | Often smaller |
| Ejaculate Volume | May be low | Usually normal |
| Genetic Testing | CFTR mutation (possible) | Y chromosome deletion (common) |
| Treatment Options | Surgical or ICSI | Hormonal, ICSI, or donor sperm |
This comparison simplifies understanding and gives clarity to treatment decisions.
Being diagnosed with azoospermia can cause emotional distress. Many men feel:
Shock or confusion
Loss of masculinity
Fear about their future as a parent
Stress within relationships
Fortunately, mental health support is now part of most fertility clinics. Counseling helps men and couples cope with emotional challenges and stay hopeful about alternative options like IVF or adoption.
Once doctors identify the cause of azoospermia, they can suggest tailored treatments. These may include:
Surgery to correct blockages
Hormone therapy for hormonal imbalances
Sperm retrieval procedures like TESE or micro-TESE
Assisted reproductive techniques such as IVF with ICSI
Donor sperm or adoption, when no sperm can be retrieved
Even though azoospermia sounds like a permanent condition, medical advancements offer many pathways to fatherhood.
Understanding how azoospermia is diagnosed empowers you to take control of your reproductive health. From semen analysis to genetic testing and biopsies, each step provides insight into what’s happening and how to move forward.
Early diagnosis matters. It not only improves treatment success but also gives couples a roadmap for navigating the emotional and medical aspects of infertility. If you suspect a problem or want to check your fertility, speak with a qualified urologist or fertility specialist.
With knowledge, support, and modern medicine, many men with azoospermia go on to achieve their dream of becoming fathers.
Q: Can azoospermia go away on its own?
A: Rarely. Sometimes temporary factors like illness or medications cause it, but most cases need medical evaluation.
Q: Is azoospermia the same as infertility?
A: Azoospermia causes infertility, but not all infertility is due to azoospermia. Some men have low sperm counts rather than none.
Q: Can doctors find sperm even if semen analysis shows none?
A: Yes. A biopsy or sperm retrieval procedure often reveals hidden sperm in men with non-obstructive azoospermia.

Introduction Male infertility, especially caused by azoospermia, affects millions of men worldwide. For those suffering from non-obstructive azoospermia, treatment options have been limited. However, thanks
Azoospermia is one of the most challenging causes of male infertility, often leaving men with few options and couples struggling to conceive. But today, an
PROLISTEM® is a Patented Formula
Copyright © 2025 Prolistem®