
Gene therapy for azoospermia treatment
Introduction Male infertility, especially caused by azoospermia, affects millions of men worldwide. For those suffering from non-obstructive azoospermia, treatment options have been limited. However, thanks
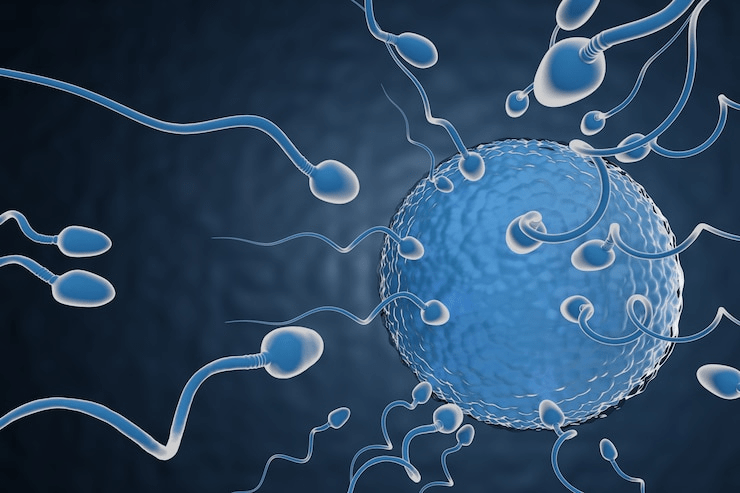
In recent years, fertility treatments have become increasingly common as more couples seek help to start a family. Among these treatments, In Vitro Fertilization (IVF) stands out as one of the most well-known and successful options. However, while much of the conversation around IVF often focuses on egg health and female fertility, sperm health is equally critical to the success of IVF procedures.
Therefore, in this article, we will explore the relationship between IVF and sperm health, why it matters, how it affects outcomes, and ways to improve sperm health before undergoing IVF.
IVF involves combining an egg and sperm outside the body in a laboratory setting. After successful fertilization, the resulting embryo is transferred to the uterus to initiate pregnancy. Consequently, the quality of both the egg and the sperm plays a pivotal role in achieving a healthy embryo and a successful pregnancy.
When discussing IVF and sperm health, it is essential to recognize that sperm quality can influence every stage of the process. From fertilization rates to embryo development and even pregnancy outcomes, healthy sperm are vital for success.
Healthy sperm contribute essential genetic material necessary for creating a viable embryo. On the other hand, poor sperm quality can lead to:
Lower fertilization rates
Poor embryo quality
Higher miscarriage rates
Increased risk of genetic abnormalities
Thus, addressing sperm health before and during IVF can significantly enhance the chances of success.
Several factors influence sperm health. Understanding these can help couples take proactive measures:
A higher sperm count increases the likelihood of successful fertilization during IVF procedures.
Motility refers to the sperm’s ability to swim toward the egg. Good motility is essential for natural conception and successful IVF.
Morphology concerns the size and shape of sperm. Notably, abnormal sperm may struggle to fertilize an egg effectively.
DNA fragmentation in sperm can result in unsuccessful fertilization, poor embryo development, or miscarriage.
Habits such as smoking, excessive alcohol consumption, poor diet, lack of exercise, and chronic stress can all negatively impact sperm health.
Issues like varicocele, infections, hormonal imbalances, and chronic illnesses can severely affect sperm production and quality.
Before starting IVF, fertility specialists usually conduct a range of tests to assess sperm health. These include:
Semen Analysis: Measures sperm count, motility, and morphology.
DNA Fragmentation Test: Assesses the integrity of sperm DNA.
Hormone Testing: Evaluates testosterone levels and other hormones related to sperm production.
Genetic Testing: Identifies potential chromosomal abnormalities that could affect embryo development.
Ultimately, understanding these results enables doctors to create a personalized IVF plan tailored to each couple’s needs.
Optimizing sperm health is crucial for improving IVF success rates. Fortunately, several evidence-based strategies can help:
A balanced diet rich in antioxidants, vitamins, and minerals supports healthy sperm production. In particular, focus on:
Fresh fruits and vegetables
Whole grains
Lean proteins
Healthy fats like omega-3 fatty acids
Supplements such as zinc, folic acid, vitamin C, vitamin E, selenium, and Coenzyme Q10 have been shown to boost sperm health.
Engaging in moderate physical activity enhances overall health and fertility. Aim for at least 30 minutes of exercise on most days.
Smoking and heavy drinking are associated with reduced sperm count and motility. Fortunately, quitting these habits can lead to noticeable improvements within a few months.
High stress levels can interfere with hormone balance and impair sperm production. Mindfulness practices, yoga, and therapy can significantly reduce stress levels.
Excessive heat, such as that from hot tubs or saunas, can damage sperm production. Wearing loose-fitting underwear and avoiding prolonged heat exposure are simple yet effective precautions.
It is crucial to diagnose and treat any underlying medical conditions that may impair sperm production.
In cases where sperm health is compromised, advanced IVF techniques can enhance outcomes:
ICSI involves injecting a single sperm directly into an egg. It is particularly helpful for men with low sperm count, poor motility, or high DNA fragmentation.
PICSI selects sperm based on their ability to bind to hyaluronic acid, helping embryologists choose mature and healthy sperm for fertilization.
IMSI uses high-magnification microscopy to select sperm with the best morphology, improving fertilization chances.
These techniques ensure that the best available sperm are utilized during IVF treatment.
Integrating lifestyle changes with IVF treatment can dramatically improve outcomes. Couples preparing for IVF should ideally commit to a fertility-friendly lifestyle at least three to six months before beginning treatment.
Both partners are encouraged to:
Eat a balanced diet
Engage in regular exercise
Quit smoking
Limit alcohol consumption
Manage stress effectively
Prioritize adequate sleep
These positive lifestyle adjustments not only benefit sperm health but also contribute to overall fertility success.
The connection between IVF and sperm health is critical when analyzing success rates. Studies consistently show that better sperm parameters correlate with higher fertilization rates, better embryo quality, and improved pregnancy and live birth outcomes.
Nevertheless, even men with poor sperm parameters can achieve success through advanced IVF techniques like ICSI. With a comprehensive approach, many couples fulfill their dream of parenthood despite initial sperm issues.
Several myths surrounding IVF and sperm health can mislead couples. Let’s clarify a few common misconceptions:
Myth 1: Only women need to worry about fertility.
Truth: Male factor infertility accounts for approximately 40-50% of infertility cases.
Myth 2: Male age does not affect fertility.
Truth: Male fertility declines with age, often impacting sperm quality and IVF outcomes.
Myth 3: Lifestyle changes do not impact fertility.
Truth: Research shows that positive lifestyle changes can significantly enhance sperm health and improve IVF results.
By dispelling these myths, couples can make more informed decisions about their fertility journey.
If conception has not occurred after a year of trying (or six months if the woman is over 35), it is advisable to consult a fertility specialist. Additionally, men with a history of:
Low sperm count
Poor motility
Previous infertility problems
Medical conditions that could affect fertility
should seek evaluation sooner. Early assessment increases the chances of successful treatment and saves valuable time.
In conclusion, IVF and sperm health are closely intertwined. High-quality sperm not only increases fertilization rates but also improves embryo development and the likelihood of a healthy pregnancy.
Men play an indispensable role in the fertility process, and improving sperm health can dramatically enhance IVF success rates. Whether through lifestyle changes, nutritional supplements, or advanced techniques like ICSI, addressing sperm health is an essential step toward achieving parenthood.
If you are considering IVF, it is vital to discuss sperm health with your fertility specialist. A holistic approach that prioritizes both egg and sperm health offers the best opportunity for a positive outcome.
Q: Can poor sperm quality affect IVF success?
A: Yes, poor sperm quality can significantly lower fertilization rates, impact embryo quality, and increase the risk of miscarriage.
Q: How long does it take to improve sperm health?
A: Sperm production typically takes about 72-90 days. Therefore, lifestyle changes should be made at least three months before undergoing IVF.
Q: What supplements help improve sperm health?
A: Zinc, folic acid, vitamin C, vitamin E, selenium, and Coenzyme Q10 are commonly recommended to enhance sperm quality.
Q: Is ICSI always necessary if sperm quality is poor?
A: Not always, but ICSI is often advised for severe sperm issues to maximize fertilization chances.
Q: Does male age affect sperm health?
A: Absolutely. Sperm quality tends to decline with age, which can impact overall fertility outcomes.

Introduction Male infertility, especially caused by azoospermia, affects millions of men worldwide. For those suffering from non-obstructive azoospermia, treatment options have been limited. However, thanks
Azoospermia is one of the most challenging causes of male infertility, often leaving men with few options and couples struggling to conceive. But today, an
PROLISTEM® is a Patented Formula
Copyright © 2025 Prolistem®