
Prolistem fertility support
Prolistem Fertility Support: Unlocking the Secrets to Enhanced Reproductive Health Many couples face challenges with conception, and infertility is more common than we often realize.
Azoospermia, the complete absence of sperm in the ejaculate, is a primary contributor to male infertility, affecting approximately 1% of all men and 10-15% of infertile men. Among these cases, non-obstructive azoospermia (NOA) accounts for about 70%. NOA arises from a failure in spermatogenesis within the testes, presenting unique challenges in fertility treatment. Recent advances, such as testicular sperm extraction (TESE) techniques, have revolutionized the ability to retrieve viable sperm, offering hope to affected individuals.
Men diagnosed with NOA often face complex fertility issues requiring innovative solutions. Conventional methods like fine needle aspiration (FNA) and traditional testicular biopsy often yield low sperm retrieval rates (SRRs). FNA, for example, retrieves sperm in only about 45% of NOA patients. Consequently, the demand for advanced techniques with higher success rates has driven the adoption of microdissection testicular sperm extraction (mTESE), now recognized as the gold standard for NOA patients.
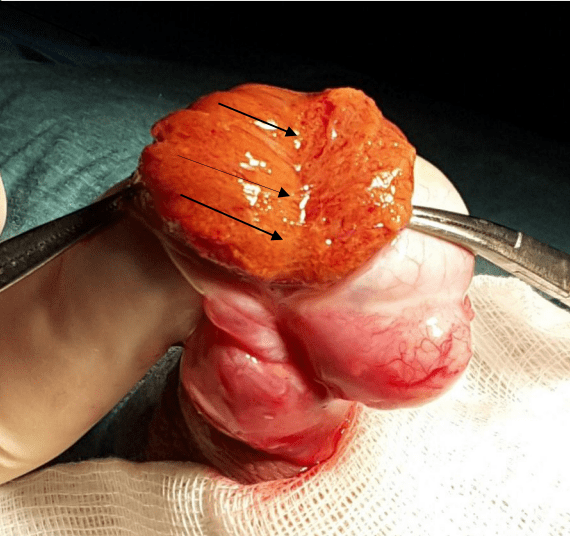
First introduced in the late 1990s, mTESE utilizes high-powered surgical microscopes to locate and extract sperm from isolated foci of spermatogenesis within the testes. Unlike random biopsies, mTESE focuses on identifying dilated seminiferous tubules, which are more likely to contain sperm. This targeted approach minimizes testicular tissue damage while achieving a higher SRR of up to 66% in some studies. Despite its efficacy, mTESE requires specialized training, equipment, and prolonged operative times, which may pose logistical and financial barriers for many centers.
To address these challenges, some institutions have developed alternative techniques using lower magnification tools, such as 6x magnifying loupes. This adaptation offers a cost-effective and accessible solution while achieving comparable SRRs. In a study spanning 14 years, a step-by-step loupe-assisted TESE procedure demonstrated an SRR of 51.8%, with sperm identified in the first testis in 61% of cases. By incorporating deep testicular dissection and real-time specimen assessment, this technique strikes a balance between efficacy and practicality.
The loupe-assisted TESE technique emphasizes precision and minimizes tissue trauma. Here’s an overview of the procedural steps:
Several factors impact the SRR in patients undergoing TESE procedures:
Pre-operative optimization can enhance TESE success rates. Patients are often advised to:
In cases of palpable varicocele, subinguinal varicocelectomy may be performed six months before TESE to improve spermatogenic conditions.
The success of loupe-assisted TESE hinges on both surgical expertise and effective collaboration with embryology teams. Surgeons must develop the skill to distinguish between dilated and non-dilated tubules, while embryologists play a crucial role in assessing retrieved specimens. In this study, a strong correlation (90%) was achieved between visual assessment and laboratory findings after a rigorous learning phase involving over 100 procedures.
Post-operative complications are rare with loupe-assisted TESE. The most common issues include mild hematomas and transient scrotal pain. Testosterone levels generally normalize within one year post-surgery. In this study, no cases of testicular atrophy were reported, highlighting the safety of the technique when performed by experienced hands.
Special attention is required for NOA patients with a history of cryptorchidism or genetic abnormalities such as AZF microdeletions and Klinefelter syndrome. In cryptorchid patients, early orchidopexy significantly improves SRRs, emphasizing the importance of timely intervention. For men with AZFc microdeletions, SRRs are typically around 55%, but hormonal optimization and early biopsy are critical to success.
Azoospermia, particularly NOA, remains a formidable challenge in male infertility. However, advances in TESE techniques, including the use of magnifying loupes, have transformed the landscape of fertility treatment. Loupe-assisted TESE offers a practical and effective alternative to mTESE, especially in resource-limited settings. By combining meticulous surgical techniques with real-time specimen assessment and pre-operative optimization, this approach maximizes the chances of successful sperm retrieval while minimizing risks.
As research continues, the development of predictive markers and enhanced protocols will further refine azoospermia treatment, offering renewed hope to countless couples worldwide.
Referance: https://pmc.ncbi.nlm.nih.gov/articles/PMC6628476/pdf/12610_2019_Article_91.pdf

Prolistem Fertility Support: Unlocking the Secrets to Enhanced Reproductive Health Many couples face challenges with conception, and infertility is more common than we often realize.

Prolistem Supplement: The Best Male Fertility Support for Azoospermia Treatment Introduction If you are struggling with male infertility, Prolistem supplement might be the solution you

Prolistem, a patented formula, has not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
Copyright © 2025 Prolistem®
Prolistem, a patented formula, has not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
Copyright © 2023 Prolistem®