My sperm count is zero how to increase
My Sperm Count is Zero – How to Increase It? Having a zero sperm count, also known as azoospermia, can be a distressing condition for
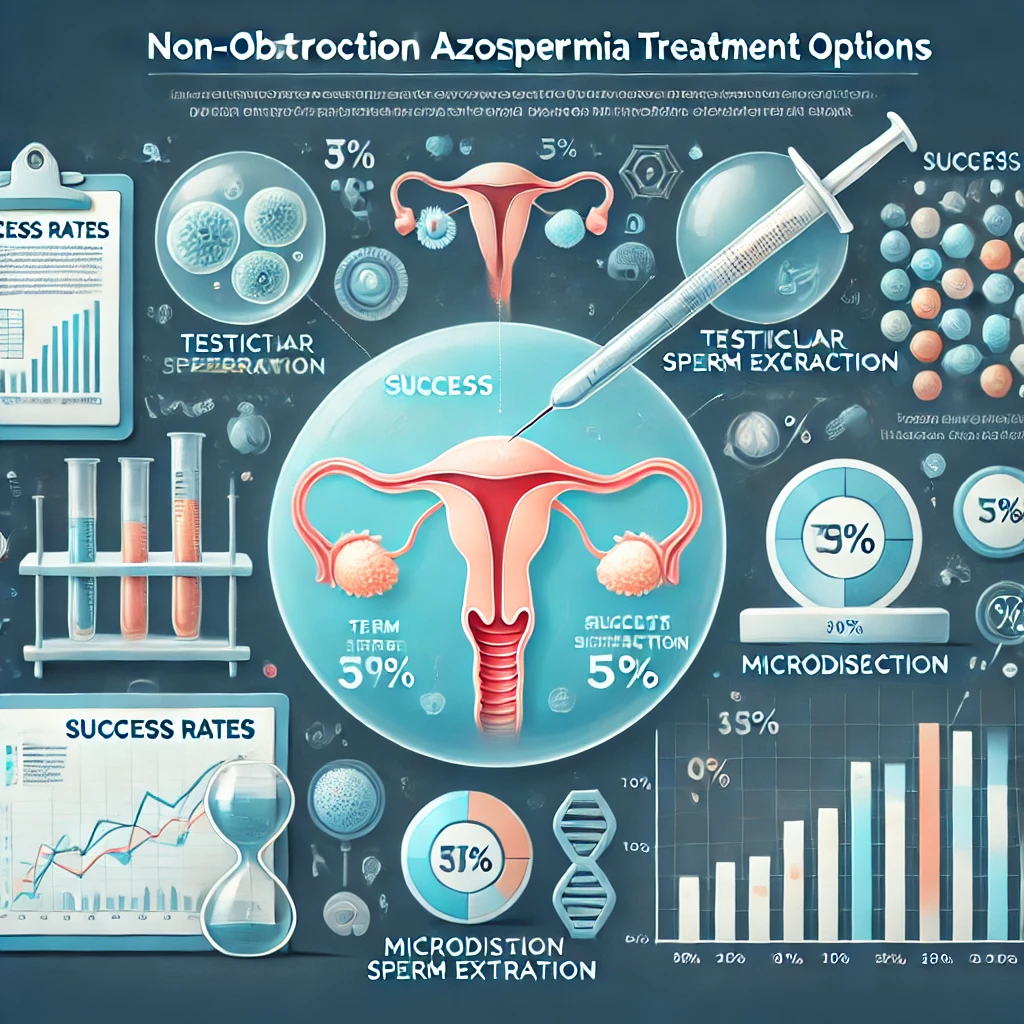
Non obstructive azoospermia success rates.Genetics of Azoospermia Infertility can be a challenging journey, and for men diagnosed with non-obstructive azoospermia (NOA), the road to fatherhood may seem uncertain. However, modern medical advancements have significantly improved azoospermia success rates, offering hope to many couples. This article explores what NOA is, the available treatments, the success rates of different methods, and ways to improve fertility outcomes.
Non-obstructive azoospermia is a severe male infertility condition where the testicles do not produce enough sperm or fail to release them into the semen. Unlike obstructive azoospermia, which is caused by blockages in the reproductive tract, NOA is usually linked to hormonal imbalances, genetic factors, or testicular failure.
Men with NOA typically do not experience noticeable symptoms other than infertility. However, some underlying causes may present with additional signs, such as:
Understanding the cause of NOA is crucial for determining treatment success. The most common causes include:
Yes! While NOA is a serious condition, many men can still have biological children through assisted reproductive techniques (ART). The key to success lies in finding viable sperm within the testicular tissue. Even when sperm is not found in the semen, advanced sperm retrieval techniques can help locate healthy sperm for fertilization.
A thorough diagnosis is essential before determining treatment options. Doctors use the following tests to diagnose NOA:
Success rates for NOA treatments vary depending on the underlying cause, patient age, and medical procedures used. Below is a detailed breakdown of the key treatment methods and their success rates:
In cases where NOA is due to hormonal imbalances, medications like Clomiphene Citrate, hCG, or FSH injections can stimulate sperm production.
ICSI is a fertilization technique used in in vitro fertilization (IVF), where a single sperm is directly injected into an egg.
If sperm is successfully retrieved through TESE or micro-TESE, the overall IVF success rate is 30-50% per cycle, with higher success in younger female partners.
If sperm retrieval fails, some couples opt for donor sperm, which has a 70-80% success rate in IVF cycles.
Men diagnosed with NOA can take additional steps to improve their chances of sperm retrieval and successful conception:
Non Obstructive Azoospermia Success. If all treatments fail, couples can explore other options such as:
A diagnosis of non-obstructive azoospermia can be emotionally challenging. It is essential to seek support and consider:
My Sperm Count is Zero – How to Increase It? Having a zero sperm count, also known as azoospermia, can be a distressing condition for
My Husband Has No Sperm – How Can I Get Pregnant? My husband has no sperm – how can I get pregnant? Discovering that your

Prolistem, a patented formula, has not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
Copyright © 2025 Prolistem®
Prolistem, a patented formula, has not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
Copyright © 2023 Prolistem®